Lumbar osteochondrosis is a chronic disease that develops as a result of a degenerative-dystrophic process in the intervertebral discs. The disease is widespread and affects most people between the ages of 25 and 40.
According to statistics, one in two adults experiences back pain at least once in their life, while in 95% of cases it is caused by osteochondrosis of the spine.
Patients with severe course of lumbar osteochondrosis, persistent pain and other manifestations are recognized as temporarily disabled. If their condition does not improve within four months, the question of creating a group of disabled people is decided.
Lumbar osteochondrosis is a serious medical and social problem, as the disease mainly affects people of working age, and in addition, if left untreated, it can lead to the formation of a herniated disc.
Causes and risk factors
The predisposing factors for the development of lumbar osteochondrosis are:
- anomalies of the structure of the spine;
- lumbarization - congenital pathology of the spine, characterized by the separation of the first vertebra from the sacrum and its transformation into the sixth (additional) lumbar; Sacralization
- is a congenital pathology in which the fifth lumbar vertebra is fused with the sacrum;
- asymmetric arrangement of the articular spaces of the intervertebral joints;
- pathological narrowing of the spinal canal;
- reflected spondiogenic pain (somatic and muscular);
- obesity;
- sedentary lifestyle;
- prolonged exposure to vibration;
- systematic physical stress;
- smoke.
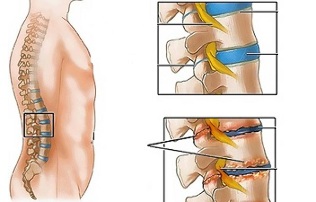
Unfavorable static-dynamic loads associated with one or more risk factors lead to a modification of the physiological properties of the nucleus pulposus of the fibrous disc, which acts as a shock absorber and ensures the mobility of the spine. This process is based on the depolymerization of polysaccharides, which leads to the loss of moisture in the gelatinous core tissue. As a result, the nucleus pulposus, and with it the fibrous disc, lose their elastic properties. Additional mechanical stress causes the annulus fibrosis to protrude, which has lost its elasticity. This phenomenon is called protrusion. Cracks appear in the fibrous nucleus, through which fragments of the nucleus pulposus fall (prolapse, herniated disc).
Prolonged compression of the nerve roots that innervate certain organs of the abdominal cavity over time leads to a deterioration in their function.
Instability of the spinal segment is accompanied by reactive changes in the body of adjacent vertebrae, intervertebral joints, and concomitant spondyloarthrosis. Significant muscle contraction, for example, against the background of physical activity, leads to displacement of the vertebral bodies and entrapment of nerve roots with the development of radicular syndrome.
Another cause of pain and neurological symptoms in lumbar osteochondrosis can be osteophytes - bone growths on the processes and vertebral bodies that cause radicular syndrome or compression myelopathy (compression of the spinal cord).
Forms of the disease
Depending on the structures involved in the pathological process, lumbar osteochondrosis is clinically manifested by the following syndromes:
- reflex- lumbodynia, lumboishalgia, lumbago; develop against the background of a reflex overload of the back muscles;
- compression (spinal, vascular, root)- compression (compression) of the spinal cord, blood vessels or nerve roots leads to their development. Examples are lumbosacral radiculitis, radiculoischemia.
Symptoms of lumbar osteochondrosis
In lumbar osteochondrosis, symptoms are determined by which structures are involved in the pathological process.
Lumbago occurs under the influence of hypothermia or physical overload, and sometimes for no apparent reason. The pain appears suddenly and is pulling in character. It intensifies when sneezing, coughing, rotating the body, exercising, sitting, standing, walking. When lying down, pain sensations are considerably weakened. Sensitivity and reflexes are preserved, the range of motion of the lumbar spine is reduced.
Observe on palpation:
- pain in the lumbar region;
- paravertebral muscle spasm;
- flattening of lumbar lordosis, which in many cases is associated with scoliosis.
Nerve root tension syndrome in lumbago is negative. When lifting a straight leg, patients notice an increase in pain in the lumbar region, and not their appearance in an extended lower limb.
Often, with lumbar osteochondrosis, there is a recurrence of pain attacks, which each time become more intense and prolonged.
In lumbodynia, the clinical presentation resembles lumbago, but the increase in pain intensity occurs over several days.
In lumboishalgia, patients complain of pain in the lumbar region, which radiates to one or both lower limbs. The pain spreads to the buttocks and the back of the thigh and never reaches the feet.
Lumboishalgia is characterized by vasomotor disorders:
- changes in temperature and color of the skin of the lower limbs;
- feeling hot or cold;
- violation of blood circulation.
The development of lumbar compression syndromes is clinically manifested by the following symptoms:
- dermatomic hypalgesia;
- shooting pains;
- weakening or complete loss of deep reflexes;
- peripheral paresis.
With compression syndromes, the pain is aggravated by flexing of the trunk, sneezing and coughing.
Diagnostics
The diagnosis of lumbar osteochondrosis is carried out on the basis of the data of the clinical picture of the disease, laboratory and instrumental research methods.
In blood tests for lumbar osteochondrosis:
- decrease in calcium concentration;
- increased ESR;
- increased levels of alkaline phosphatase.
In the diagnosis of lumbar osteochondrosis, great importance is attached to the x-ray examination of the spine.
Prolonged compression of the nerve roots that innervate certain organs of the abdominal cavity over time leads to a deterioration in their function.
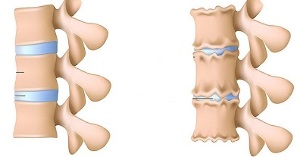
The radiographic signs which confirm the diagnosis are:
- modify the configuration of the affected segment;
- pseudospondylolisthesis (displacement of adjacent vertebral bodies);
- deformation of the closure plates;
- flattening of the intervertebral disc;
- uneven height of the intervertebral disc (symptom of a spacer), associated with asymmetric muscle tone.
Are also used in the diagnosis of lumbar osteochondrosis, if present:
- myelography, magnetic or calculated resonance imaging - are necessary for persistent symptoms, the development of neurological deficits;
- scintigraphy (study of the accumulation of phosphorus in the bone system, marked with tech-99) - is carried out when there is a suspicion of a tumor or infectious process, spinal cord injury.
The differential diagnosis of lumbar osteochondrosis is carried out with the following diseases:
- spondylolisthesis;
- dyshormonal spondylopathy;
- ankylosing spondylitis (ankylosing spondylitis);
- infectious process (inflammation of the disc, spinal osteomyelitis);
- neoplastic processes (primary tumor of the spine or its metastatic lesions);
- rheumatoid arthritis;
- deforming osteoarthritis of the hip joint;
- reflected pain (diseases of internal organs and large blood vessels).
Treatment of lumbar osteochondrosis
For lumbar osteochondrosis, the following treatment tactics are usually followed:
- bed rest for 2-3 days;
- traction of the affected segment of the spine;
- strengthening of back muscles and abdominal muscles (creation of the so-called muscle corset);
- impact on myofascial and myotonic pathological processes.
Lumbago occurs under the influence of hypothermia or physical overload, and sometimes for no apparent reason.
In most cases, conservative treatment of lumbar osteochondrosis is performed, including:
- infiltration anesthesia of the muscles with a solution of local anesthetics;
- take nonsteroidal anti-inflammatory drugs;
- taking desensitizing agents; vitamin therapy
- ;
- taking tranquilizers and antidepressants;
- manual therapy, massage;
- physiotherapy exercises;
- acupuncture;
- post-isometric relaxation.
The absolute indications for surgical treatment of lumbar osteochondrosis are:
- acute or subacute spinal cord compression;
- development of cauda equina syndrome, characterized by dysfunction of the pelvic organs, sensory disturbances and movement.
Therapeutic exercises for lumbar osteochondrosis
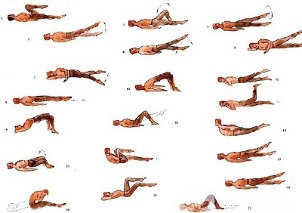
Physiotherapy plays an important role in the complex treatment of lumbar osteochondrosis. Regular exercises allow you to normalize the muscle tone of the paravertebral muscles, improve metabolic processes in the tissues affected by the pathological process, and in addition to forming a well-developed muscle corset that can support the spine in the right position, inrelieve unnecessary static charges.
In order for gymnastics for lumbar osteochondrosis to produce the most effect, the following principles should be observed:
- regularity of the classes;
- gradual increase in the intensity of physical activity;
- avoid overworking in class.
Physiotherapy should be carried out under the guidance of an experienced instructor, who will select the most effective exercises for a particular patient and check the correctness of their implementation.
According to statistics, one in two adults experiences back pain at least once in their life, while in 95% of cases it is caused by osteochondrosis of the spine.
In addition to classes with an instructor, you need to perform a series of morning exercises daily, which includes special exercises for lumbar osteochondrosis.
- Relaxation and contraction of the abdominal muscles.The starting position is standing, feet shoulder-width apart, arms lowered to the body. Take a gentle breath as you relax the muscles of the anterior abdominal wall. While exhaling, pull the stomach as much as possible, engaging the abdominal muscles. The exercise should be repeated until the appearance of slight fatigue.
- Movements of the head with spinal flexion.The starting position is kneeling, resting on the floor with outstretched arms, back straight. Slowly raise your head and lean behind your back. Hold this position for a few seconds, then slowly return to the starting position. Repeat at least 10 to 12 times.
- "Pendulum".The starting position is lying on your back, arms at your sides, legs bent at a right angle at the knees and hips. Rotate your legs to the right and left in swinging movements, trying to reach the ground. In this case, the shoulder blades cannot be torn off the ground.
- Boat.Starting position lying on your stomach, arms extended forward. Rip your upper body and legs off the ground while leaning behind your back. Hold this position for 5-6 seconds and slowly return to the starting position. Run 10 times.
Consequences and potential complications
The main complications of lumbar osteochondrosis are:
- formation of intervertebral hernia;
- vegetative-vascular dystonia;
- spondylolysis, spondylolisthesis; osteophytosis
- ;
- spondylarthrosis;
- Spinal stenosis, which causes compression of the spinal cord and can lead to permanent disability and reduced quality of life.
Prolonged compression of the nerve roots that innervate certain organs of the abdominal cavity over time leads to a deterioration in their function. As a result, patients present with intestinal (constipation, diarrhea, flatulence) and pelvic (urinary disorders, erectile dysfunction, frigidity, infertility) dysfunctions.
Forecast
Pain syndrome in lumbar osteochondrosis occurs in the form of remissions and exacerbations. Lumbago lasts 10-15 days, after which the patient's condition improves, the pain subsides. A favorable outcome can be avoided by associated secondary diseases. Often with lumbar osteochondrosis there is a recurrence of pain attacks, which each time become more intense and prolonged.
Physiotherapy plays an important role in the complex treatment of lumbar osteochondrosis.
Patients with severe course of lumbar osteochondrosis, persistent pain and other manifestations are recognized as temporarily disabled. If their condition does not improve within four months, the question of creating a group of disabled people is decided.
Prevention
Prevention of the development of osteochondrosis of the spine consists of the following measures:
- quit smoking;
- normalization of body weight;
- improvement in general physical condition, active lifestyle;
- avoid provocative conditions (lifting weights, sudden movements, turns, turns).












































